Measles Outbreak Surges Across the U.S., Surpassing 2024’s Total Cases in Just Three Months
With over 292 cases reported in Texas and New Mexico alone, health officials warn of rising infections in major cities amid growing anti-vaccine sentiment.
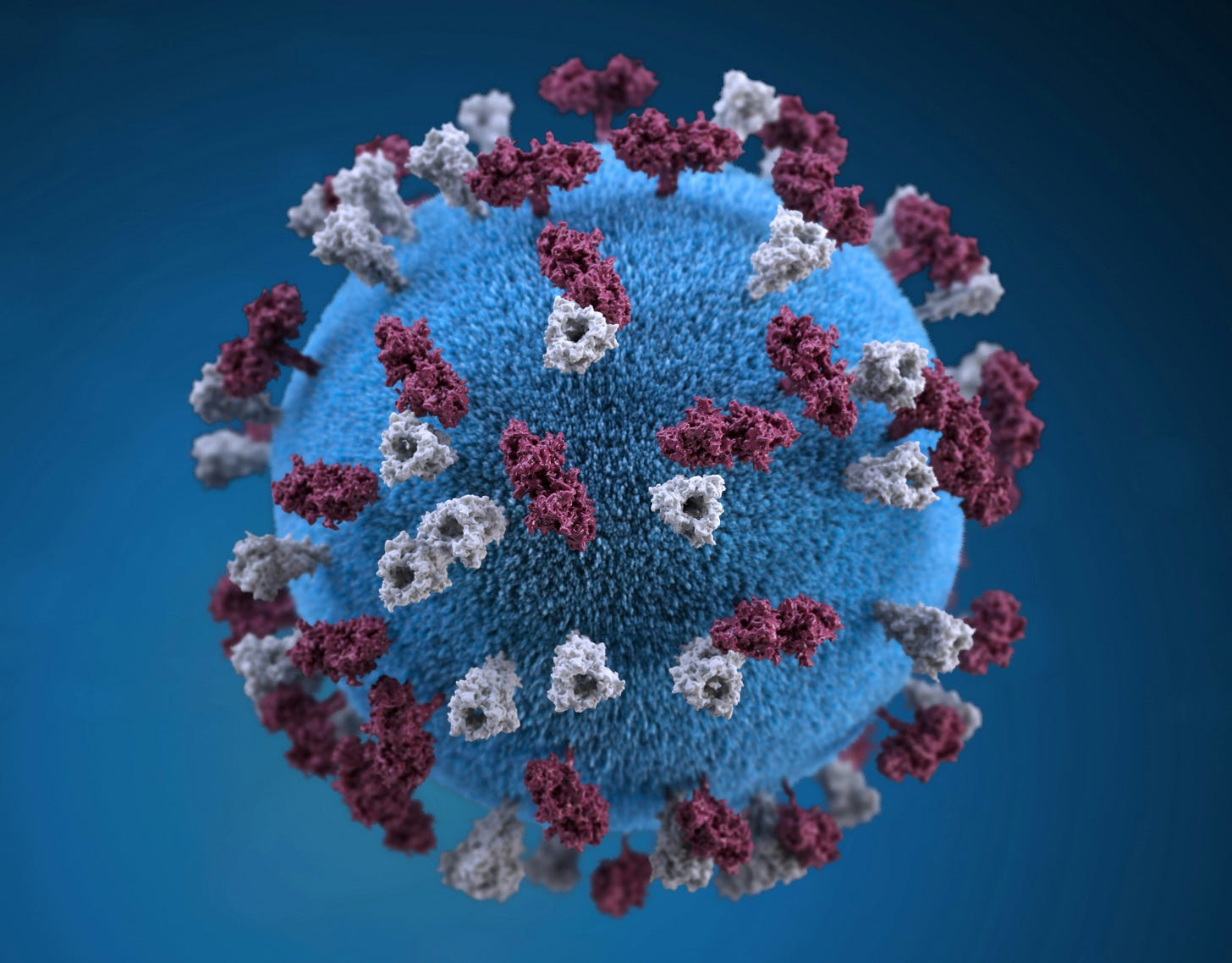
Originally declared eliminated in the United States in 2000, measles is experiencing a major resurgence as anti-vaccine sentiment grows. The virus, also known as rubeola, causes high fever, rash, cough, and red eyes. Life-threatening complications, including brain inflammation and pneumonia, can also occur.
According to the Centers for Disease Control and Prevention (CDC), more than 300 measles cases have been reported across the United States, including in Texas, New York, Pennsylvania, New Mexico, California, and Maryland. The current outbreak has already exceeded last year’s total, which itself marked an increase from 2023. Two deaths have been reported, highlighting growing concerns as vaccination rates fall below the 95% threshold needed to control the spread of the virus.
The Current State of the Outbreak
Texas has been hit the hardest by the current outbreak, with more than 279 confirmed cases in the state. The majority of those affected are unvaccinated, and the largest impacted age group is children and teenagers between 5 and 17.
“Due to the highly contagious nature of this disease, additional cases are likely to occur in the outbreak area and the surrounding communities,” the Texas Department of State Health Services (DSHS) said in a press release.
Most of the state's cases have been reported in the South Plains and Panhandle regions of western Texas. One unvaccinated child with no prior health complications became the first person in the state to die from the outbreak—the first measles-related death in the United States since 2015. Health officials expect the virus to continue spreading due to its highly contagious nature.
“This is going to be a large outbreak, and we are still on the side where we are increasing the number of cases,” said Katherine Wells, director of Lubbock Public Health, in a report by CNN.
“I’m really thinking this is going to be a year long.”
In New Mexico, more than 33 cases have been reported, primarily in Lea County, which borders Texas. The second death in the outbreak occurred in New Mexico after a resident tested positive for the virus posthumously.
“The official cause of death is still under investigation by the New Mexico Office of the Medical Investigator. However, the NMDOH Scientific Laboratory has confirmed the presence of the measles virus. The individual did not seek medical care before passing,” the New Mexico Department of Health (NMDOH) said in an update.
The person was also believed to be unvaccinated, according to state officials monitoring the outbreak.
“Any measles diagnosis is a concern, and we are watching every case closely,” said Dr. Miranda Durham, chief medical officer of NMDOH, in a statement.
“We are heartened by the number of New Mexicans getting vaccinated in response to this outbreak.”
According to the same report, more than 9,000 New Mexicans have received the measles, mumps, and rubella (MMR) vaccine this year, compared with 5,342 vaccinations at the same time last year.
Meanwhile, data from The New York Times shows that cases are spreading beyond the South and Southwest, with infections reported in Kentucky, Vermont, Rhode Island, Pennsylvania, and Washington state. Cities detecting new cases include Los Angeles, Miami, Atlanta, New York City, and Baltimore.
Vaccine Hesitancy and Anti-Vax Movements
With measles vaccination rates falling below the threshold needed to control the disease, a rising anti-vaccine sentiment is spreading throughout the U.S. This trend has been influenced by vaccine misinformation and disinformation, as well as public health concerns following the confirmation of Robert F. Kennedy Jr. as secretary of Health and Human Services, as detailed in a previous report by The Introspective.
Studies show that since the start of the COVID-19 pandemic, various states have seen declines in vaccination rates and increases in exemption rates. During the 2023-24 school year, fewer than 93% of kindergarten students received required vaccines such as the measles, mumps, and rubella (MMR) vaccine; diphtheria, tetanus, and acellular pertussis (DTaP) vaccine; polio vaccine; and varicella vaccine—down from 95% during the 2019-20 school year. Research from the Office of Disease Prevention and Health Promotion (OASH) indicates that the MMR vaccination rate has fallen below the 95% level needed to prevent community transmission of measles, falling short of the projected 2030 goal. As a result, more than 280,000 children remain unvaccinated and vulnerable to the disease, raising concerns as the majority of measles’ 100,000 global fatalities are children.
“It is one of the most infectious diseases that we have,” said Dr. Lucia Donatelli, a member of the Center for Immunization, Infectious Disease Epidemiology, and Outbreak Response Bureau at the Maryland Department of Health, in an interview with CBS Baltimore.
“There’s a 90% secondary attack rate. If you’re not fully immunized against measles, there is a 90% chance that if you’re exposed, you will contract measles. That’s why it’s so important for everybody to be vaccinated.”
According to the same report, most people in the United States are immune to measles because they have either been vaccinated, recovered from the virus, or were born before 1957.
“One dose of the MMR vaccine is 93% effective in preventing measles. Two doses are 97% effective,” Donatelli said.
The outbreak in Texas allegedly began in Gaines County, which is now the state’s epicenter. Reports from The Associated Press highlight that nearly 14% of children through 12th grade in the county had a vaccine exemption during the 2023-24 school year—five times the state average of 2.32% and higher than the national average of 3.3%.
Concerns about measles have also spread to Canada, where outbreaks have begun occurring. More than 173 infections have been reported in Ontario in recent weeks.
“I think we do have areas and school districts where there are enough unprotected children that measles could take off if it gets introduced here,” said Caroline Colijn, a Canada 150 Research Chair at Simon Fraser University, in a report by CBC.
According to the same report, over 90% of 7-year-olds in British Columbia were vaccinated against measles in 2013, but by 2023, that number had declined to 72.4%—a 17.6% drop in 10 years.
Health officials such as Jia Hu, medical director for immunization programs at the British Columbia Centre for Disease Control (BCCDC), noted that vaccination rates may appear lower due to residents not being registered in the province’s immunization database. However, he acknowledged that the rates are below the level needed to prevent the spread of measles, which was eliminated from Canada in 1998.
“I also think, more worryingly, that there probably has been a decline in people’s willingness to get a measles-containing vaccine—or any vaccine, for that matter,” Hu said.
“In the aftermath of the pandemic, we’ve seen a lot more vaccine hesitancy.”
Before the measles vaccine was introduced in 1963, between 400 and 500 children died from the disease annually in the United States.
Public Health Response
As health officials respond to the outbreak, many hospitals in rural Texas are struggling to manage the increase in patients.
“If we see the volume of patients exceed the number of beds available at children’s hospitals, we’re going to need a contingency plan,” said Melanie Richburg, chief executive officer of the Lynn County Hospital District, in an interview with the Texas Tribune.
“The biggest struggle we have is the same struggle we had during COVID.”
The pandemic highlighted disparities in urban and rural health care. Data from the Texas Department of Agriculture shows that more than 64 counties in Texas lack a hospital, and over 25 have no primary care physicians. A report from the Texas Organization of Rural & Community Hospitals (TORCH) found that more than 26 rural hospitals closed in Texas between 2010 and 2020, with many of those remaining facing staff shortages and deteriorating infrastructure.
Additional research underscores the urban-rural health care divide. Rural residents are more likely to live in food deserts—areas with limited access to affordable, nutritious food—and are less likely than their urban counterparts to have health insurance.
In a report by NPR, doctors emphasized the importance of vaccination, citing the long-term effects of measles.
“He got the virus from a child in his neighborhood who was unvaccinated,” said Dr. Alex Cvijanovich, referring to a 20-year-old case of a 7-month-old who contracted measles and recovered but later developed complications in middle school. The child was later diagnosed with subacute sclerosing panencephalitis (SSPE), a rare and fatal neurological condition that emerges seven to 10 years after infection.
“The problem is that there is no treatment for it,” Cvijanovich said.
“And he basically became more and more incapacitated over time.”
The teenager died 18 months after his diagnosis.
Since the outbreak began, the Centers for Disease Control and Prevention (CDC) has issued a travel advisory for Texas and New Mexico, warning travelers ahead of the summer season.
“With spring and summer travel season approaching in the United States, CDC emphasizes the important role that clinicians and public health officials play in preventing the spread of measles,” the agency said in a statement, urging people to remain “vigilant” for potential symptoms.
“They should be vigilant for cases of febrile rash illness that meet the measles case definition and share effective measles prevention strategies, including vaccination guidance for international travelers.”
The resurgence of measles highlights ongoing challenges in public health, from vaccine hesitancy to disparities in rural health care. As officials work to contain outbreaks, the response to this crisis may shape future vaccination policies and preparedness efforts across the country.






It’s so sad that people are willing to risk their kids lives over lies they were fed and believed. Those poor kids who don’t have a choice